The Office of the State EMS Medical Director (OMD) provides leadership and coordination for state medical programs, protocols, and quality assurance in Maryland’s EMS system. In addition, the Aeromedical Director, Associate State EMS Medical Director for Pediatrics, and Regional EMS Medical Directors for each of the five regions collaborate with the State EMS Medical Director to update the Maryland Medical Protocols for Emergency Medical Services on an annual basis. Regional EMS Medical Directors also assist the Jurisdictional EMS Medical Directors in each of Maryland’s 28 jurisdictional EMS operational programs with protocol implementation and quality assurance initiatives. Fourteen of Maryland’s EMS Medical Directors are board-certified in EMS medicine. A network of 49 EMS base stations located in emergency departments provide online medical direction through Emergency Medical Resource Center and Systems Communications (EMRC/SYSCOM). The Office of the State EMS Medical Director ensures that patients who interact with the Maryland EMS system receive consistent, high-quality out-of-hospital medical care.
Phone: 410-706-0880 |
Fax: 410-706-0853 (fax).
Maryland EMS Protocols
To reflect best practices and evidence-based medicine and define appropriate EMS evaluation and treatment, The Maryland Medical Protocols for Emergency Medical Services are updated annually with expert review and approval by the Protocol Review Committee. This committee incorporates multidisciplinary input from medical directors, emergency physicians, nurses, and EMS clinicians from across the state.
The following are significant additions and modifications to The Maryland Medical Protocols for Emergency Medical Services effective on July 1, 2025:
- Adult High-Performance CPR: This change incorporates high-performance CPR principles within the BLS Adult Cardiac Arrest Algorithm. The separate High-Performance CPR protocol in the Procedures section has been removed.
- Alcohol Withdrawal Protocol: This revision incorporates the use of midazolam for treatment of moderate and severe alcohol withdrawal. Determination of withdrawal severity is based upon the Brief Alcohol Withdrawal Scale (BAWS).
- Calcium Chloride: For consistency, calcium chloride administration times for adult patients have been changed to 3-5 minutes for all indications.
- Cefazolin: This new protocol adds an antibiotic, cefazolin, for treatment of patients with open fractures, amputations, and mangled or degloved extremities. Changes are reflected in the Multiple/Severe Trauma, Hand/Upper and Lower Extremity Trauma, and ALS Pharmacology sections.
- Cold-Related Emergencies: This modification adds a provision for rapid transport of hypothermic cardiac arrest patients to an Extracorporeal Cardiopulmonary Resuscitation (ECPR)-capable hospital if the facility is within 30 minutes.
- Dexamethasone: The maximum dose of dexamethasone increases from 10 mg to 15 mg for adult and pediatric patients to reflect dosing recommendations for respiratory conditions in the medical literature.
- Drowning: This modification updates the Near-Drowning Protocol to meet current clinical practices and terminology. Rather than drowning and near-drowning, the classifications are now submersion injury and submersion injury with cardiac arrest. Termination of resuscitation criteria, based upon submersion time and water temperature, have been added, as have transport guidelines that include considerations for transport to ECPR-capable hospitals.
- Droperidol: This modification of the ALS Droperidol Pharmacology adds Intramuscular (IM) as an acceptable route of droperidol administration for treatment of nausea and vomiting. The requirement for a medical consultation for administration of diphenhydramine in the event of a dystonic reaction has been removed.
- High-Consequence Infectious Diseases (HCID) Procedure: These revisions update the prior Emerging Infectious Diseases (EID) procedure to incorporate current practices and terminology. The protocol outlines a broader framework that may be applied to novel diseases, rather than being Ebola-specific. • Hypertensive Disorders of Pregnancy: This new protocol provides treatment guidelines for moderate-to-severe gestational hypertension and preeclampsia, as well as modifications to the existing treatment of eclampsia. Labetalol has been added to the ALS Pharmacology for treatment of severe hypertension. Indications for magnesium sulfate have been expanded to include treatment of moderate and severe hypertension and the frontline treatment of eclamptic seizures.
- Intraosseous Infusion Procedure: This modification adds the distal femur as an approved insertion site for pediatric patients. A reference chart that shows preferred IO site by age is included.
- V Infusion Pump Pharmacology Optional Supplemental Protocol (OSP): This revision adds sodium bicarbonate to the IV Infusion Pump Pharmacology section.
- Naloxone “Leave Behind” Protocol: The Naloxone “Leave Behind” Protocol moves from an optional supplemental protocol to standard EMS treatment protocol within the Overdose/Poisoning section.
- Pediatric Tachycardia Algorithm: Medical consultation is required for cardioversion of pediatric patients with 9 narrow complex tachycardia. This revision ensures consistency with the consultation requirement for cardioversion of regular wide-complex tachycardia.
- Removal of Unused Pilot and Optional Supplemental Protocols (OSP): The Vascular Doppler Device Pilot Protocol and the Mobile Integrated Health: COVID- 19 Monoclonal Antibody Administration Optional Supplemental Protocol have been removed due to lack of current use.
- Sepsis – Adult: These modifications incorporate the earlier use of vasopressors in the treatment of adult patients who are severely hypotensive or “volume sensitive” (CHF, ESRD). These modifications have also been added to the Shock: Hypoperfusion – Adult Protocol.
- Tranexamic Acid (TXA): The administration time has been reduced from 10 minutes to 3-5 minutes.
- Transport to Freestanding Emergency Medical Facility Optional Supplemental Protocols (OSP): The Transport to Freestanding Medical Facility at Aberdeen Optional Supplemental Protocol and Transport to Freestanding Medical Facility (Base Station or Non-Base Station) Optional Supplemental Protocol have been combined.
- Video Laryngoscopy for Orotracheal Intubation: Video laryngoscopy moves from being an optional supplemental protocol into standard EMS treatment protocol. EMS operational programs must have video laryngoscopy capability no later than July 1, 2026.
- Wilderness EMS Optional Supplemental Protocols (OSP): These updates provide consistency with current practices and the standard EMS treatment protocols. Substantive changes include: the addition of hypertonic saline for treatment of acute exercise-induced hyponatremia (with medical consultation); doxycycline administration to pediatric patients for prophylactic treatment of tick bites; and targeted MAP readings for patients with spinal trauma.
Maryland EMS Protocol Page
Regional Medical Directors
MIEMSS coordinates a network of Regional EMS medical directors, who serve as the principal medical advisors for their respective regional councils, hospitals in the region, and jurisdictional medical directors. As members of the MIEMSS Protocol Review Committee, these physicians propose new protocols and revisions to existing protocols. They assist the jurisdictional medical directors with QA/QI and support educational efforts, with a particular focus on new protocol implementation. In conjunction with the MIEMSS Office of Clinical Integration and MIEMSS Regional Coordinators, the Regional EMS medical directors conduct hospital base station site surveys. They also assist the State EMS medical director with the development of base station education and credentialing of hospital base station instructors.
Regional Programs Page
EMS Medical Directors by Region:
| Region I |
Janelle Martin, MD |
| Region II |
Jeffrey Fillmore, MD |
| Region III |
Matthew Levy, DO, MSc, FACEP, FAEMS |
| Region IV |
Thomas Chiccone, MD, FACEP |
| Region V |
Roger Stone, MD |
Hospital Base Stations
EMS base stations are a critical component of Maryland EMS. Base stations provide real-time support and guidance to EMS clinicians in the field. There are 49 Maryland hospital base stations designated by the State EMS Board.
Physicians and nurses who answer base station calls are required to successfully complete the MIEMSS Base Station Communications Course for Emergency Department Personnel and the Maryland EMS Updates for Hospital Base Station Personnel training video to ensure they are prepared to communicate with EMS clinicians to provide real-time medical consultation. From July 2024 through June 2025, as a result to multiple hospitals facilitating the base station course and the addition of 11 instructors, MIEMSS issued 513 base station certificates to emergency physicians and nurses.
Hospital Base Station's Page
eMEDS® - electronic Maryland EMS Data System
The electronic Maryland EMS Data System (eMEDS®) is one of the few statewide comprehensive prehospital patient care reporting systems in the United States. eMEDS® relies on an ImageTrend® software product that complies with the latest standards set by the National Emergency Medical Services Information System (NEMSIS). MIEMSS holds a statewide site license for eMEDS®, offering it at no cost to local jurisdictions. All Maryland jurisdictional EMS operational programs (JEMSOPs) and approximately 20% of commercial ambulance companies submit patient care reports directly into eMEDS®, while most commercial service reports are automatically imported into eMEDS® from thirdparty electronic health platforms. All Maryland healthcare facilities have access to the prehospital patient care reports through the Hospital Hub online application. eMEDS® supports several key goals, including:
- Uniform Data Collection: Ensures consistent reporting of prehospital care by Maryland’s EMS clinicians.
- Performance Measurement: Provides a basis for evaluating patient care and compliance with protocols by local departments, EMSOPs, regional medical directors, and MIEMSS. • Standardized Reporting: Facilitates compliant data reporting to the National EMS Information System (NEMSIS).
- Data Integration: Supports integration with statewide systems such as Electronic Surveillance System for the Early Notification of Community-based Epidemics (ESSENCE), Chesapeake Regional Information System for Patients (CRISP), Overdose Detection Mapping Application Program (ODMAP), Maryland Trauma Registry, Cardiac Arrest Registry to Enhance Survival (CARES), Emergency Department Advisory System (EDAS), and MIEMSS’ eLicensure System. • Local EMSOP Integration: Includes integration with 9-1-1 center computer-aided dispatch (CAD) systems, exports to third-party billing vendors for reimbursement, and data sharing with third-party vendors for local reporting, dashboard creation, and fire incident reporting.
- Maintaining and Updating EMS Systems: Updated to version 3.5 in 2023, eMEDS® 3.5.1 is under review for implementation to maintain NEMSIS compliance.
 eMEDS® Mobile Integrated Health (MIH) Module
eMEDS® Mobile Integrated Health (MIH) Module
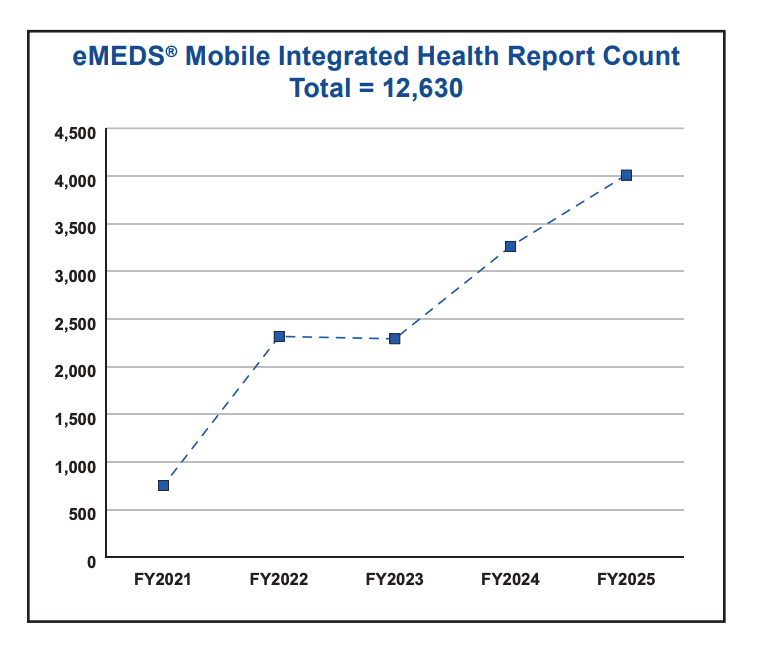
MIEMSS continues to support enhancements to the eMEDS® Mobile Integrated Health (MIH) module, developed in 2020, to improve data collection and guide future MIH efforts. As of the end of FY 2025, over 12,100 reports have been recorded using the MIH module. Starting in FY 2024, MIEMSS began working with CRISP to export MIH data to the state’s designated health information exchange.
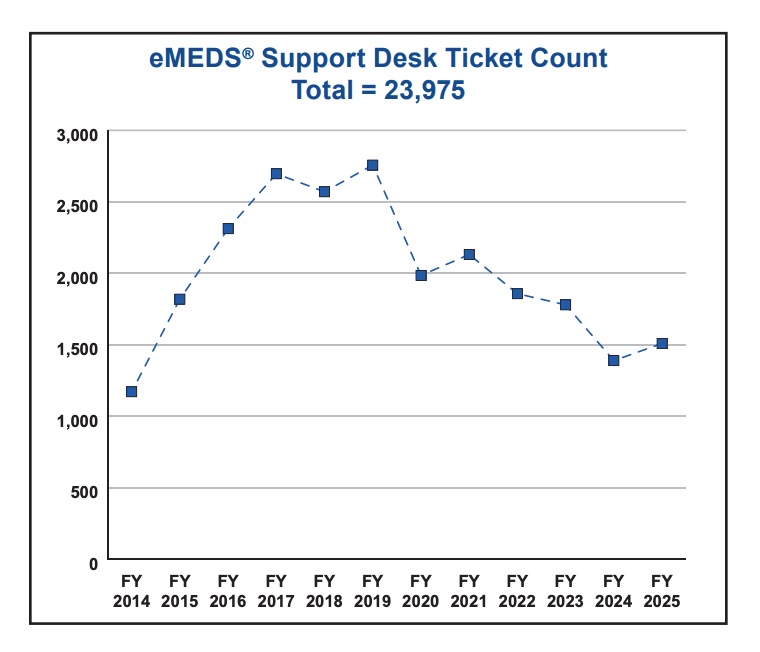 eMEDS® Support Desk (emeds-support@miemss.org) The eMEDS® application includes a MIEMSS support desk that handles requests from EMS clinicians, EMS Operational Program (EMSOP) administrators, and healthcare facility personnel across the state. Common issues include password resets, login problems, access level questions, report writer functionality, EMSOP integrations, and general application inquiries. During FY 2025, the support desk processed over 1,500 support tickets.
eMEDS® Support Desk (emeds-support@miemss.org) The eMEDS® application includes a MIEMSS support desk that handles requests from EMS clinicians, EMS Operational Program (EMSOP) administrators, and healthcare facility personnel across the state. Common issues include password resets, login problems, access level questions, report writer functionality, EMSOP integrations, and general application inquiries. During FY 2025, the support desk processed over 1,500 support tickets.
eMEDS® Statewide Steering Committee Jurisdictional, commercial, and hospital stakeholders continue to meet on a quarterly basis to discuss topics for eMEDS® improvement. Topics include system-wide integrations, enhancements, and change requests. To address continual improvement, change requests for the eMEDS® application can be submitted by any stakeholder who uses or interacts with the system. The committee reviews requests and supports actions for implementation.
eMEDS® Page | ImageTrend®,
Cares Program
MIEMSS works with the Cardiac Arrest Registry to Enhance Survival (CARES) in order to measure and ultimately improve emergency cardiac care in Maryland. CARES is an out-ofhospital cardiac arrest registry for the United States, facilitating uniform data collection and quality improvement in each state and nationally.
With the updated and consolidated Cardiac Arrest tab in eMEDS®, the statewide prehospital patient care reporting system, EMS clinicians can readily enter comprehensive prehospital cardiac arrest information. MIEMSS can then export the prehospital information directly to CARES when it is first entered, saving time for clinicians and EMS CARES coordinators. Using a single patient care record for CARES submission makes Maryland one of the first states to incorporate this process within their electronic patient care reporting documentation. Maryland hospitals then enter outcome data into the CARES report for those cardiac patients who receive ongoing care in the ED.
Cares Program Page
EMS Medical Directors’ Symposium
The 30th EMS Medical Directors’ Symposium is designed to increase statewide collaboration and the promotion of state-of-the-art techniques in the field for Emergency Services. The 30th Annual EMS Medical Directors’ Symposium, held April 9, 2025, at the James Robey Public Safety Training Center in Marriottsville, MD, was attended by regional, jurisdictional, and commercial ambulance services medical directors, highest jurisdictional EMS officials, quality assurance officers, and MIEMSS personnel.
Cardiac Arrest Steering Commitee
The Cardiac Arrest Steering Committee (CASC), as authorized by the State EMS Board, provides guidance to MIEMSS’ medical and executive leadership teams on matters related to sudden cardiac arrest in Maryland. The committee actively works on matters related to public health and safety by sharing best MEDICAL DIRECTION 8 practices regarding telecommunicator CPR, prehospital cardiac arrest management performance improvement, and further development of a comprehensive statewide system for the treatment of sudden cardiac arrest. In FY 2025, CASC introduced several new members to its roster, including emergency clinicians, 9-1-1 administrators, and pediatric champions, and empowered four subcommittees to continue efforts to improve cardiac arrest survival through 9-1-1 and EMS synergy and community engagement.
Updated 10-1-2025